Keywords: Hand surgery; wrist; carpectomy; scaphoid; lunate dislocation
Authors: Jorge Jimenez Lopez, MD; Anastasia Boptsi, MD; Konstantinos Kalousis, MD Institution: Universitätsklinikum Schleswig-Holstein Lübeck
Abstract
Carpal dislocation fractures are uncommon injuries, most frequently associated with high-energy trauma. Combined carpal dislocations without associated bone fractures are even rarer. Delayed treatment can have serious consequences. The case presented here involves an 86-year-old man with dislocation of the scaphoid and lunate bones, as well as acute carpal tunnel syndrome resulting from the injury. PRC is mostly a salvage operation but given the severity of ligamentous disruption, the need to restore the patient’s mobility and also the fact, that scaphoid was irreducible, a proximal row carpectomy (PRC) was performed to preserve wrist range of motion (ROM).
Patient medical history
The 86-year-old patient crashed the car into the wall of his garage at a speed of 30 km/h. As a result, the patient presented a dislocation of the lunate bone and the scaphoid. The patient lived alone and was completely independent. Regarding other conditions, he suffered from arterial hypertension and prostate cancer.


Before and After
Patient examination
There was a visible deformity at the right wrist with bruising, and swelling. Additionally, a positive Hoffman-Tinel sign was observed with paresthesia in the median nerve area. A radiological examination of the hand was then performed, which revealed a dislocation of the scaphoid and lunate bones. No bone fractures were detected.
Pre-operative considerations
Given the severity of ligamentous disruption and the need to restore the patient’s mobility a proximal row carpectomy (PRC) was performed to preserve wrist range of motion (ROM).
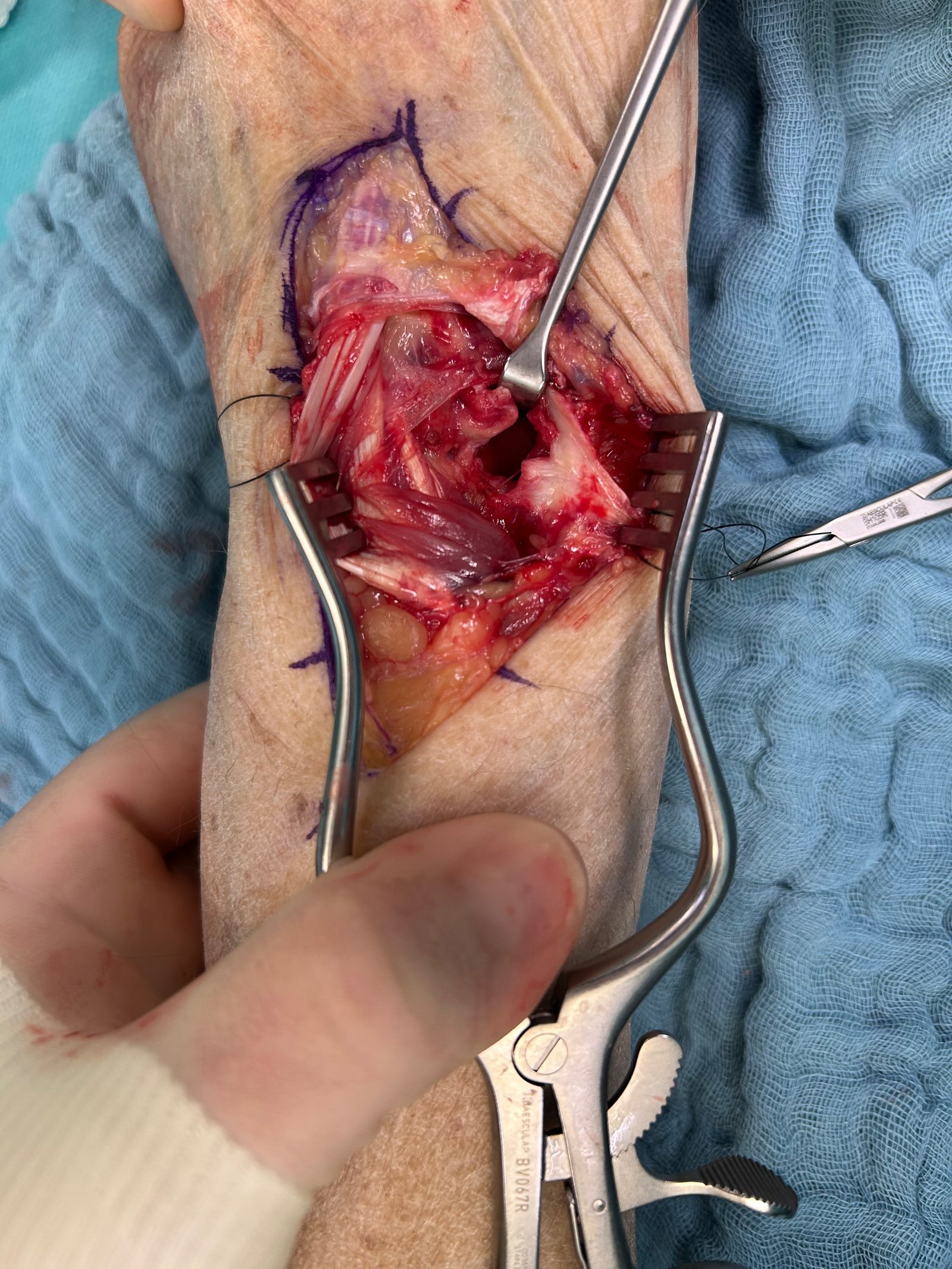
Surgical Dorsal Exposure
The surgical procedure involved exposing and splitting the 4th and 3rd extensor tendon compartments to facilitate access. The extensor pollicis longus (EPL) tendon was transposed subcutaneously, and the extensor tendons were luxated out of the 4th extensor tendon compartment. The posterior interosseous nerve was identified and divided. Additionally, the dorsal joint capsule was found to be torn, and the scaphoid and lunate bones were luxated ventrally, with the lunate bone rotated 90°

Palmar Approach, Carpal Tunnel Release and Neurolysis of the Median Nerve
A skin incision was made along the Linea vitalis, extending proximally to the distal forearm. The palmar aponeurosis, flexor brevis muscle (which was coagulated), and the flexor retinaculum were divided. The median nerve was exposed and underwent neurolysis, and the palmar branch of the median nerve was also identified and neurolyzed. Both the median nerve and the flexor tendons were retracted to the side. The palmar joint capsule was found to be torn. The scaphoid and lunate bones were displaced into the carpal tunnel. A carpal tunnel release was performed. The lunate and scaphoid bones were only secured by the ventral ligaments. The remaining ligaments, including the SL and LT ligaments, were torn. The lunate and scaphoid bones were then resected from the palmar side.

Proximal Row Carpectomy
Further steps were performed dorsally, including the resection of the triquetral bone. The second row of carpal bones was then moved proximally, forming a new joint between the capitate bone and the lunate fossa. The joint was mobilized. An impingement was observed during radial abduction, so the tip of the styloid process of the radius was resected using an oscillating saw. The joint capsule was closed both palmar and dorsal using PDS 2.0 continuous sutures. The extensor retinaculum was closed using PDS 3.0 continuous sutures.

Good immediate result
The postoperative result was controlled under X-ray, showing full range of motion of the wrist in all planes, with normal articulation of the capitate bone at the lunate fossa.
Pearls
Pay attention to impingement with the radius
Pitfalls
To avoid complications, we recommend carefully selecting the patient and assessing all aspects before making a surgical decision. Additionally, the procedure should be performed by an experienced hand surgeon. We also recommend intensive physiotherapy to prevent stiffness.
Post-operative plan
Immobilization in a splint for 6 weeks and physiotherapy performed without the splint.
References
- Campano, D. et al. (2024) ‘Dorsal lunate dislocation and en bloc proximal row carpectomy: A case report’, Journal of Surgical Case Reports, 2024(2). doi:10.1093/jscr/rjae043.
- Kennedy, S.A. and Allan, C.H. (2012) ‘In brief: Mayfield et al.. classification: Carpal dislocations and progressive perilunar instability’, Clinical Orthopaedics & Related Research, 470(4), pp. 1243–1245. doi:10.1007/s11999-012-2275-x.
- Muller, T. et al. (2017) ‘Treatment of acute perilunate dislocations: ORIF versus proximal row carpectomy’, Orthopaedics & Traumatology: Surgery & Research, 103(1), pp. 95–99. doi:10.1016/j.otsr.2016.10.014.
- Jerome, T.J. and Prabu, G.R. (2021) ‘Proximal row carpectomy for complex perilunate fracture dislocations with migration of proximal scaphoid bone into the forearm’, Hand Surgery and Rehabilitation, 40(3), pp. 299–304. doi:10.1016/j.hansur.2020.12.002.
- Della Santa, D.R. et al. (2010) ‘Proximal row carpectomy in emergency’, Chirurgie de la Main, 29(4), pp. 224–230. doi:10.1016/j.main.2010.06.001.