Keywords: bilobed flap, larger facial skin defects, cheek reconstruction, reconstructive surgery
Authors: Sahar Vanessa Amiri (MD) and Matilda Svenning Hunt (MD). Institution: Department of Plastic Surgery and Burns, Rigshospitalet, Denmark
Abstract
This case describes the use of a bilobed flap for reconstruction of a large cheek defect following excision of a squamous cell carcinoma in an 86-year-old male. Due to the tumor size and previous surgical scarring, direct closure was not feasible. The bilobed flap was chosen as the preferred reconstructive approach because of its ability to provide adequate coverage of the defect while allowing for primary closure of the donor site. Postoperative follow-up at three months demonstrated satisfactory aesthetic outcomes, with no wound complications or recurrence.
Patient medical history
The patient, an 86-year-old male diagnosed with hypertension, paroxysmal heart flutter, and with a history of carcinoma, was referred to us with a large, localized tumor on the right cheek. According to the patient’s history, the tumor had been present for more than one year. The biopsy showed squamous cell carcinoma, and the histological subtype was unspecified. On clinical examination, the tumor was described as 20*25*6 mm, localized on the parotid gland, and clinically not adherent to the underlying tissue. The patient had a scar from a previous full-thickness skin graft (FTSG) on the right temple. There were no palpable regional lymph nodes. The patient was operated on under local anesthesia. Because of the size of the tumor, direct closure was not feasible. Local flaps were deemed a preferred reconstruction method. The tumor was excised with a 7 mm safety margin and depth excision margin to SMAS (Superficial Musculoaponeurotic System). Histology from frozen sections showed no malignancy.


Before and After
Patient examination
The patient presented with significant sun damage and poor skin quality. The tumor was 20 x 25 mm in diameter and elevated 6 mm from the skin surface. It was approximately one centimeter anterior to the tragus and showed no adherence to the underlying tissue upon palpation.
The patient had several scars from previous operations, including a full-thickness skin graft on the right temple.
Pre-operative considerations
The bilobed flap is a versatile and reliable local flap that provides excellent aesthetic outcomes. This technique offers an effective approach for reconstruction of not only nasal defects, but also larger skin defects on other areas of the face.
The bilobed flap was chosen as the preferred reconstructive approach because of its ability to provide adequate coverage of the defect while allowing for primary closure of the donor site. Additionally, the defect was located away from the central facial region, minimizing the visibility of scarring upon healing from the selected donor site. Furthermore, the patient had sufficient tissue laxity in the caudal regions, particularly around the submandibular and cervical areas IIa and IIb (1).

SCC excision and flap design
After excision with a 7 mm safety margin and frozen sections with no malignancy, the resulting defect was measured at 40 × 34 mm. When designing a bilobular flap, the interrelation between the lobes is crucial. The first lobe should consist of a semicircular flap positioned adjacent to the defect. Ideally, this flap should form a 45-degree angle to the defect; however, in this case, a larger angle was necessary due to the width of the defect. The diameter of the first lobe should correspond to that of the defect. In this case, the diameter of the first lobe is slightly smaller than the defect, making use of the surrounding skin`s laxity.
Fact: *The bilobed flap was first described by Esser in 1918 and has since then been modified several times, among others by McGregor and Zitelli. It is commonly used for nasal defects (2).

Anatomy
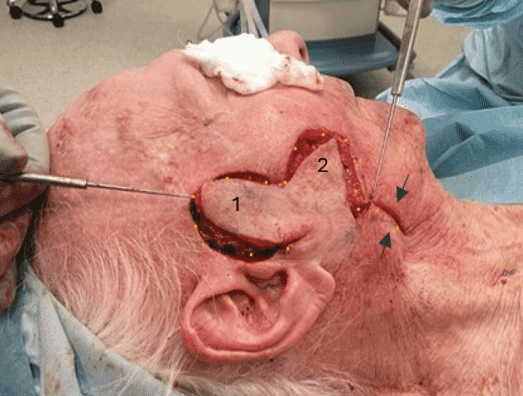
When operating on the face, it is essential to maintain a consistent plane and carefully consider the anatomical structures in the region. In the accompanying image, the two arrows indicate critical underlying anatomical structures: the temporal branch of the facial nerve and the parotid gland.
Based on the size of the defect and the planned incision pattern, the incision was initiated at the base of the defect. Careful subcutaneous dissection was performed.

Anatomy – Illustration
This drawing presents facial soft tissue layers, highlighting key structures involved in facial surgery and reconstruction.

The bilobed flap continued
The second lobe is an adjacent flap, here modified to extend nearly 180 degrees from the defect, following the original design (2,3). The diameter is three-quarters that of the first lobe and is designed to rotate into the space previously occupied by the first lobe.
Accurate measurement of the radius is crucial.
The distance from the defect’s center to its base should match the distance to the pivot point.
Transposition of the flap
The dissected flap was transposed into the defect using surgical hooks, as demonstrated in the image. Excess skin excision was not considered necessary. Defect 2 (donor site) is closed first (marked with arrows).
Fact: *The bilobed flap is classified as a random-pattern transposition flap.

Flap inset

One week follow-up
One week post-operatively
The patient presented with slight discoloration; however, the flap had fully healed with normal capillary response. The patient had no complaints.

3 months postoperative follow-up
At the three-month post-operative follow-up, the patient presented with a satisfactory cosmetic outcome. The flap was fully healed, without any wound dehiscence or signs of recurrence. A partial frontal palsy of the frontal branch of the facial nerve was encountered upon physical examination. This is likely a result of local nerve lesion during surgical excision due to tumor growth, and a watchful waiting had been chosen in agreement with the patient.
Pearls
Pitfalls
Post-operative plan
Due to poor skin quality and perioperative debris from the skin, the patient was placed on a five-day course of prophylactic antibiotics. Postoperatively, the patient was instructed to keep the head elevated and to avoid applying pressure to the right cheek. Additionally, the patient was advised to refrain from consuming hot food and beverages on the first postoperative day. Strenuous physical activities, including sports and household chores, were also discouraged until suture removal.
References
- 1. Steele, R. , Jellinek, N. , Foy, A. , Lee, K. , Vij, A. & Knackstedt, T. (2020). Use of Ex-tranasal Bilobed Transposition Flaps in Cutaneous Reconstructive Surgery at 2 Institu-tions. Dermatologic Surgery, 46 (10), 1279-1285. doi: 10.1097/DSS.0000000000002319.
- 2. Lal T, Lal J. Bilobed Flaps: An Esthetic Method of Reconstructing Circular Defects. J Cutan Aesthet Surg. 2023 Jul-Sep;16(3):245-251. doi: 10.4103/JCAS.JCAS_168_22. PMID: 38189074; PMCID: PMC10768961.
- 3. McGregor John C, A clinical assessment of the bilobed flap. PII: S0007-1226(81)80094-X
- 4. Esser J. Gestielte locale Nasenplastik mit zweizipfligem Lappen, Deckung des se-kundaren Defktes vom ersten Zipfel durch den Zweiten. Dtsch Z Chir 1918;385–90.