Keywords: Rectus Diastasis, Plication, Abdominoplasty, following pregnancy
Authors: Theresia Skytte Eriksen, Helle Sjøstrand and Ida Felbo Pold. Institution: Department of Plastic Surgery, Herlev and Gentofte Hospital, Denmark
Abstract
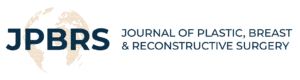
38-year-old woman underwent plication of symptomatic diastasis of the rectus abdominal muscles after twin-birth by caesarean section. The diastasis had a maximal width of 6,6 cm just above the umbilicus and her symptoms included core-instability, back-pain, and a feeling of being unprotected around her abdomen especially while handling her children.
Patient medical history
38-year-old woman had after twin-birth developed symptomatic diastasis of the rectus abdominal muscles. She had no comorbidities. She had an older child of 6 years, and the twins were 2 years old. All children were delivered by uncomplicated caesarean section. The patient described symptoms as back-pain, nausea, core instability, discomfort during running, and pain when encountering pressure to the abdomen especially while handling the children. Physical rehabilitation with physiotherapists had not been successful and hard to complete do to discomfort and pain.

Before and After
Patient examination
The patient was initially examined 15 months postpartum and at an additionally examination two years postpartum by the same surgeon.
A preoperative CT-scan at 15 months postpartum, showed a rectus diastasis with the maximal width of 6,6 cm just above the umbilicus. The objective examination confirmed those findings, and a small umbillical hernia was detected. No change in symptoms and width of the diastasis was found between the two examinations.
Pre-operative considerations
Physical training alone has not been found to reduce the width of the diastasis [1]. Surgery was in one randomized controlled trial superior to physical training with regard to reduction of pain and increase abdominal muscle strength [2]. The swedish guidelines currently recommend that surgery is indicated if the diastasis is greater than 5 cm and symptomatic. In case of severe symptoms, a diastasis as low as 3 cm can indicate the need for surgery [3]. With that in mind a surgical plication of the diastasis was considered to be the optimal treatment for this patient.
The patient was informed of the possible complications related to surgery as bleeding, infection, scarring, sensory disturbances, tissue necrosis, placement of suction drain, lift of pubic hair, and asymmetric cosmetic result because of loose skin.
Furthermore, the patient must not have a wish for future pregnancy, and it is recommended that at least 2 years has passed since the latest pregnancy, in order to comply with post-op restrictions.

Perioperative drawing of the loose abdominal skin before incision
The perioperative drawings are made in a standing position estimating the amount of loose skin expected to be excised.

Incision and undermining of the abdominal skin
Incision was made according to the caudal drawing and the skin was undermined at the plan of the fascia. The flap was raised up to 2-3 cm under the curvature of the ribs.
Perioperative drawing and measurement of the diastasis of the rectus abdominal muscles
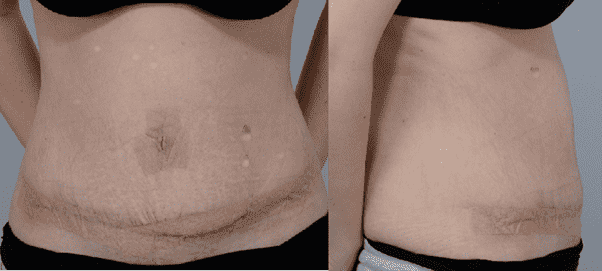
The maximum width was measured to 6,5 cm. The diastasis stretched from 1 cm below proc. xiphoideus to 4 cm above the symphysis.

Plication of the rectus diastasis and around the umbilicus (Illustration)
The small umbilical hernia only contained fat which was excised and the defect in the fascia was closed with 3-0 Vicryl.
The plication of the diastasis was made with PDS 0 Loop-suture as a continuous suture. The suture was continued around the umbilicus. Starting cranially, locking the suture in the loop. At the end of the plication, one tread was cut and the two sutures were knotted together. The knot and suture ends were buried in the tissue.

Removal of the extensive loose skin to tighten up the abdomen
Carefully measurement of the amount of extensive loose skin which can be surgically removed, so that the incision could be closed without too much tension. Approximately 550g of skin tissue was removed.

Closure of the incision and re-placement of the umbilicus
After thorough hemostasis the new hole for the umbilicus was made with a diamond-shaped incision. The umbilicus was sutured to the skin with 3-0 Novosyn and 5-0 Prolene.
The distal incision was closed in 3 layers with 2 layers of 3-0 Novosyn in the depth and the skin intracutaneously with 3-0 Biosyn.
Tranexamic acid were administrated both intravenously and in diluted state directly into the cavity.
A suction drain, and pain regulating catheter was placed. 8 ml of ropivacaine 7,5 mg/ml was administrated by the catheter at the end of the surgery. All incisions were covered by micropore tape.
The patient was discharged two days later.

2 weeks post-op.
The patient was seen two weeks postoperatively for suture removal around the umbilicus. There was no sign of infection, and no patient-reported pain. On the lower left side, a small seroma formation was detected.
Pearls
Pitfalls
Post-operative plan
References
- [1] S. B. Gluppe, M. Ellström Engh, and K. Bø, “Curl-up exercises improve abdominal muscle strength without worsening inter-recti distance in women with diastasis recti abdominis post-partum: a randomised controlled trial,” J Physiother, vol. 69, no. 3, pp. 160–167, Jul. 2023, doi: 10.1016/j.jphys.2023.05.017.
- [2] P. Emanuelsson, U. Gunnarsson, U. Dahlstrand, K. Strigård, and B. Stark, “Operative cor-rection of abdominal rectus diastasis (ARD) reduces pain and improves abdominal wall mus-cle strength: A randomized, prospective trial comparing retromuscular mesh repair to double-row, self-retaining sutures,” Surgery (United States), vol. 160, no. 5, pp. 1367–1375, Nov. 2016, doi: 10.1016/j.surg.2016.05.035.
- [3] A. Carlstedt et al., “Management of diastasis of the rectus abdominis muscles: recommenda-tions for swedish national guidelines,” Sep. 01, 2021, SAGE Publications Inc. doi: 10.1177/1457496920961000.
- [4] G. G. Nervil et al., “Simple plication alleviates physical symptoms in patients with post-gestational rectus diastasis,” Hernia, vol. 27, no. 4, pp. 957–968, Aug. 2023, doi: 10.1007/s10029-023-02814-y.